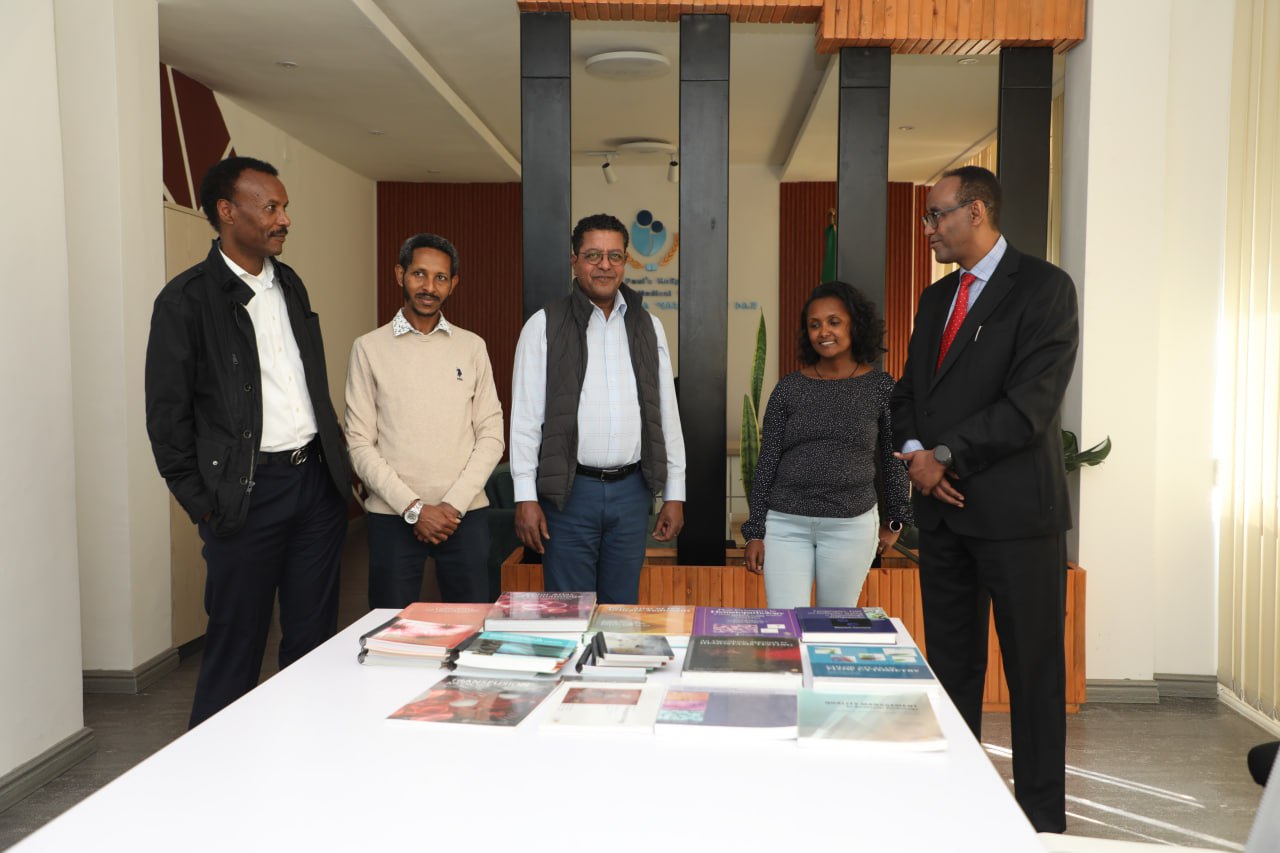
Mulugeta Gebregziabher, PhD
Professor and Vice Chair
Department of Public Health Sciences
Medical University of South Carolina
E-mail: gebregz@musc.edu
Introduction: An electronic medical record (EMR) is the systematized collection of electronically-stored demographics and health information (e.g., medical history, medications, test results, billing data, etc.) on patients in a digital format [1]. EMR systems are designed to store data accurately in searchable digital form to capture the state of a patient across time with key advantages that include (i) elimination of the need to track down a patient’s previous paper medical records allowing data to be accurate and legible; (ii) reducing data replication; (iii) extracting medical data to assess trends and long term changes in a patient; (iv) facilitating population-based studies. Countries have the choice of developing in-house software platform, purchasing commercial software, or opting for an open-source depending on the overall cost of the respective system and the value it adds to an existing paper-based system. In this short report, a comparative analysis of commercial systems and open-source systems to establish EMRs is provided in a resource-limited setting like Ethiopia. This, in its own way, can spur an on-going debate in the programmatic developments of setting up an electronic health information systems (eHIS) in Ethiopia and beyond.
A literature review on EMR systems was conducted by searching major databases such as the Scopus (which includes MEDLINE and Embase), African Index Medicus, and IEEEXplore. Journal articles and conference proceedings, including ahead-of-print articles published in English from 2000 to 2018 (August) focusing on Ethiopia, Kenya, Rwanda, Tanzania, Mozambique, Uganda, Ghana, Botswana, Sierra Leone, South Africa were retrieved . The search strategy identified 1,103 citations. Studies that were published before 2000, written in a language other than English, or were not accessible without a fee were excluded. The winnowing process resulted in 35 final articles that were deemed relevant to the objectives of this report. The summary of the results of what systems to exist in these African countries is given in Table 1.
Table 1. Summary information about EHR systems in selected sub-Saharan African countries
| Country | EHR system | Year introduced | World Bank Classification by Income type | Open-source or Commercial? |
| Ethiopia | Variety of local systems | 2009 | Low | Both |
| Kenya | OpenMRS | 2006 | Low-middle | Open-source |
| Tanzania | OpenMRS | 2008 | Low | Open-source |
| Uganda | OpenMRS | 2006 | Low | Open-source |
| Rwanda | OpenMRS | 2006 | Low | Open-source |
| Ghana | Variety of local systems | Not known | Low-middle | Both |
| Botswana | MEDITECH | 2005 | Upper-middle | Commercial |
| Sierra Leone | OpenMRS | 2014 | Low | Open-source |
| South Africa | OpenMRS, MEDITECH | 2006, | Upper-middle | Open-source |
| Mozambique | OpenMRS | 2008 | Low | Open-source |
Commercial systems: Some of the most commonly used commercial EHR systems include Epic, Cerner, MEDITECH, and InterSystems [2]. These commercial systems are mostly used in the United States, Europe, Latin America and to some extent in the Middle East, but not in SSA (need to expand SSA) countries with the exception of MEDITECH. MEDITECH South Africa Ltd has been operating in Southern African countries (South Africa, Botswana, and Namibia). The low penetration of commercial EHR vendors in Africa can be attributed to the substantial cost that is incurred [3]. Other challenges include: (i) product lifespan to ensure that vendors and products are long-lasting; and (ii) the vendor’s reliability for product customization to avoid further expenses. Out-of-the-box functionality may not meet all the requirements in a given setting. However, commercial systems have certain key advantages that make them attractive. Implementations typically require minimal programmer/configuration personnel [2, 3]. Vended products usually undergo extensive testing prior to rollout, provide warranties and liability insurance, and most importantly, vendors provide system support and maintenance, including updates, bug-fixes, security patches, and feature enhancements [2,3].
Open-source systems: Open-source software (OSS) allows users to adopt, modify, and redistribute the software subject to a number of possible license options [4]. OSS is developed by a community of volunteer programmers and it is a model for open collaboration [5]. There are several types of open source licenses. The prominent ones are approved by the Open Source Initiative (OSI), www.opensource.org. OSI-approved licenses have strong communities and are listed in the aforementioned link. Table 2 provides a comparative analysis open-source and commercial systems. It shows how much great care is necessary when identifying and selecting a reliable EHR system.
Table 2: Comparative and qualitative summary for commercial and open-source EHR systems
| Commercial | Open-Source |
| High cost and mostly used in developed countries | Cost effective and mostly used in low-resource settings |
| Focused on revenue and profit | Focused on collaboration and volunteering |
| Support can be readily available for as long as the vendor is in business | Support can be limited since volunteers normally need to attend to another full-time role |
| Limited room for feature enhancements | Flexible for feature enhancements |
| Easier to implement with full vendor support | Needs skilled implementers |
| Rarely built to have inter-operability with other systems | OSS are mostly designed with the future including interoperability |
| Provides warranties, liability insurance, bug fixes and resolution of security issues | No warranties or liability insurance, and may take time to resolve bug or security issues |
| High system cost on top of infrastructure, hardware and personnel costs makes it challenging to scale up at national level | Free of charge system helps scale up at national level – infrastructure, hardware and personnel costs still applicable |
Status of EHR in Ethiopia: To date, no EHR system has been nationally deployed in Ethiopia. Some efforts to deploy EHR within referral hospitals occurred at a few universities. For example, SmartCare, a hybrid EHR system which has been running at Ayder Referral Hospital in Mekelle. A study on SmartCare across five hospitals in Ethiopia indicated some challenges with the implementation of this system [6], including the lack of dedicated IT support at a given site and double documentation (paper-based and EHR) causing dissatisfaction and inconsistency.
Another EHR system, WHONET, is a free Windows-based database software developed for the management of laboratory data, with a focus on antimicrobial susceptibility test results [7]. WHONET has been available since 1989 through the World Health Organization (WHO) Collaborating Centre for Surveillance of Antimicrobial Resistance based at the Brigham and Women’s Hospital in Boston. The system is used by clinical, public health, veterinary, and food laboratories in over 90 countries to support local and national surveillance programs. Currently, WHONET is being piloted in four sites in Ethiopia (Ayder Hospital in Mekelle, Tikur Anbessa Hospital in Addis Ababa, Ethiopian Public Health Institute in Addis Ababa, and a fourth center in Dessie).
iCare is a newer EHR systems developed by the Ministry of Science and Technology in Ethiopia, with the goal of developing a national EHR system. In 2018, iCare was piloted at Tikur Anbessa Hospital in Addis Ababa. No performance assessment of this system has occurred yet. It is too early to document the level of acceptance of iCare by the main Ethiopian stakeholders, including the Ministry of Health of the Federal Democratic Republic of Ethiopia. Similarly, an open-source EHR system with limited application in Ethiopia is the OpenMRS with Bahmni, which includes a laboratory management system (OpenELIS) that was implemented at the Leishmaniasis Research and Treatment Centre at the University of Gondar, Ethiopia [8].
Considerations for choosing an EHR system
Scalability, interoperability, and flexibility to add new features: Most commercial systems are developed by companies who are in competition for business. These systems normally can be scalable, but they may lack the interoperability and flexibility that are required in a national healthcare system strategy. Reliable open-source systems are not pre-defined and are developed by a global community of experts supported by major non-governmental organizations (NGOs). Such an approach has led to the creation of open-source EHR systems that are scalable, interoperable with other open-source systems such as DHIS2, and flexible for adding new features. Scaling up the EHR system at the national level involves building a power and connectivity infrastructure, improving security to support safely storing electronic equipment, designing paper encounter forms, installing servers, designing electronic forms, and setting up workstations.
Cyber support through information and communications technology communities: A reliable internet connection is essential for remote access and support by experts. A commercial provider may want to monitor system stability after installation, support issues that may arise, or engage remotely in other activities. Internet reliability is even more important for open-source systems because most experts are located globally, and regular communication is required from conception to implementation. Findings from a study on mobile health for low-resource settings highlight the need to counter the loss of local knowledge and capable personnel through brain-drain by establishing international collaboration among information and communications technology (ICT) professionals in five areas: health information systems, telemedicine, mHealth, eLearning and public information [9].
Security and privacy: Security and privacy could present concerns when adopting an EHR system [10,11]. The following administrative, physical, and technical themes have been identified for safeguarding EHR security: risk analysis and management, availability of a chief information security officer, system security evaluation, and appropriate personnel for certain roles, contingency issues, business continuity planning, and disaster recovery planning. Physical safeguards involve assigning security responsibility, physical access control, and workstation security, as well as implementing radio frequency identification (RFID). The technical aspects of security and privacy include access control, entity authentication, data encryption, audit trails log, firewall protection, and malware monitoring. A separate study [11] indicates the need to train healthcare workers in security and privacy.
Financing: A study of low-resource settings showed that financing should not be a major criterion for EHR success. In addition to clinical benefits to improve the quality of healthcare [12] in low-resource settings, EHR systems can bring financial benefits [13] by shortening patient hospital length of stay, reducing transcription time, and improving laboratory utilization efficiency. Financing for EHR system is normally required for a pilot scheme and scaling up to the national level. There are various ways to finance a pilot study including federal or regional government budgets, as well as grants from one or more NGOs with established relationships with policy makers.
Infrastructure and hardware requirements: To ensure available lifesaving information in an Ethiopian EHR, the underlying hardware requires a redundant power supply. The ideal power system will have a primary power source (such as grid power or solar) and a secondary source (such as a generator or solar), both feeding into short-term backup batteries [14]. The required server hardware specifications depend on the size of the healthcare institution and the number of patients who will be supported. For example, OpenMRS requires 1.5+ GHz, 2 GB of memory, and 150+ GB of disk space with a redundant array of independent disks (RAID) and appropriate backup facilities to support 100,000 patients. Client workstations are connected to the servers over a LAN or WLAN infrastructure. Workstations, laptops, and mobile devices may be used at the point of care.
Personnel requirements: The design of OpenMRS uses a tiered architecture for the layers and components [14]. Thus, experts who have the knowledge of the whole technical stack (such as server maintenance, MySQL, Tomcat, and Java) are required for successful implementation and maintenance of the system. Ideally, two to four full-time software engineers should be involved during the implementation phase, which may take several months. Familiarity with clinical form design and dictionary design are critical. A dedicated IT support will be required for maintenance of any implemented system.
Conclusion and Recommendations: Whether to implement an open-source or commercial EHR system in resource-limited settings has been debated for several years. However, evidence that clearly demonstrates the advantages of one system over another is lacking in SSA. This comprehensive literature review helps to fill the gap. Lessons learned, as well as opportunities, challenges, and best practices for current EHR systems in SSA and specifically in Ethiopia have been identified. This review shows that while OpenMRS is the most commonly-used EHR open-source system in SSA, MEDITECH, a commercial system, is also entering African markets. Thus, an open source system with a robust capacity development program could be considered as the best approach for the Ethiopian setting.
Acknowledgement: This article is a synopsis of a collaborative manuscript that is under review and the author would like to thank his co-authors Ezana Haile, Tewelle Wellemariam, Teri Lynn Herbert, Jihad S. Obeid.
Disclaimer: The author has no conflict of interest with any of the companies discussed in this manuscript. This article represents the views of the author.
References
[1] Gunter, T.D., Terry, N.P., (March 2005), The emergence of national electronic health record architectures in the United States and Australia: models, costs, and questions, Journal of Medical Internet. Research 2005, 7 (1): e3.DOI:10.2196/jmir.7.1.e3. PMC 1550638. PMID 15829475.
[2] De la Torre Díez, I., Martínez-Pérez, B. and López-Coronado, M., Analyzing open-source and commercial EHR solutions from an international perspective, IEEE 15th International Conference on e-Health Networking, Applications and Services (Healthcom 2013) 2013, pp. 399-403, DOI: 10.1109/HealthCom.2013.6720708.
[3] Johnson III, R.J., A Comprehensive Review of an Electronic Health Record System Soon to Assume Market Ascendancy: EPIC®, J Healthc Commun. 2016, 1:4. DOI: 10.4172/2472-1654.100036.
[4] St. Laurent, Andrew, M., Understanding Open Source and Free Software Licensing, O’Reilly Media 2008, p. 4. ISBN 9780596553951.
[5] Levine, S.S., Prietula, M.J., Open Collaboration for Innovation: Principles and Performance, Organization Science 2013, 25 (5): 1414–1433. arXiv:1406.7541 Freely accessible. DOI:10.1287/orsc.2013.0872. ISSN 1047-7039.
[6] Tilahun, B., Fritz, F., Comprehensive Evaluation of Electronic Medical Record System Use and User Satisfaction at Five Low-Resource Setting Hospitals in Ethiopia, JMIR Med Inform. 2015, 3(2):e22. DOI: 10.2196/medinform.4106.
[7] Agarwal, A., Kapila, K., Kumar, S., WHONET Software for the Surveillance of Antimicrobial Susceptibility, Med J Armed Forces India 2009 Jul, 65(3): 264–266. Published online 2011 Jul 21. DOI: 10.1016/S0377-1237(09)80020-8.
[8] Syzdykova, A., Zolfo, M., Malta, A., Diro, E., Oliveira, J.L., Customisation of OpenMRS for the Leishmaniasis Research and Treatment Centre in Ethiopia, Int Soc Telemed eHealth 2017, 5(GKR):e65.
[9] Madore, A., Rosenberg, J., Muyindike, W.R., Bangsberg, D.R., Bwana, M.B., Martin, J.N., Kanyesigye, M., Weintraub, R., Implementation of electronic medical records requires more than new software: Lessons on integrating and managing health technologies from Mbarara, Uganda, Healthcare 2015, 3 (4), pp. 264-269.
[10] Kumar, P., Paton, C., Kirigia, D., I’ve got 99 problems but a phone ain’t one: Electronic and mobile health in low and middle income countries, Archives of Disease in Childhood 2016, 101 (10), 974-979.
[11] Fernández-Alemán, J.L., Señor, I.C., Lozoya, P.Á., Toval, A., Security and privacy in electronic health records: A systematic literature review, J Biomed Inform. 2013 Jun, 46(3):541-62. DOI: 10.1016/j.jbi.2012.12.003. Epub 2013 Jan.
[12] Muthee, V., Bochner, A.F., Osterman, A., Liku, N., Akhwale, W., Kwach, J., Prachi, M., Wamicwe, J., Odhiambo, J., Onyango, F., Puttkammer, N., The impact of routine data quality assessments on electronic medical record data quality in Kenya, PLoS ONE 2018, 13 (4).
[13] Driessen, J., Cioffi, M., Alide, N., Landis-Lewis, Z., Gamadzi, G., Gadabu, O.J., Douglas, G., Modeling return on investment for an electronic medical record system in Lilongwe, Malawi, Journal of the American Medical Informatics Association 2013, 20 (4), pp. 743-748.
[14] Wolfe, B.A., Mamlin, B.W., Biondich, P.G., Fraser, H.S., Jazayeri, D., Allen, C., Miranda, J., Tierney, W.M., The OpenMRS System: Collaborating Toward an Open Source EMR for Developing Countries, AMIA Annu Symp Proc. 2006, 2006:1146.